Retina / Retinal Detachment
What is retinal detachment?
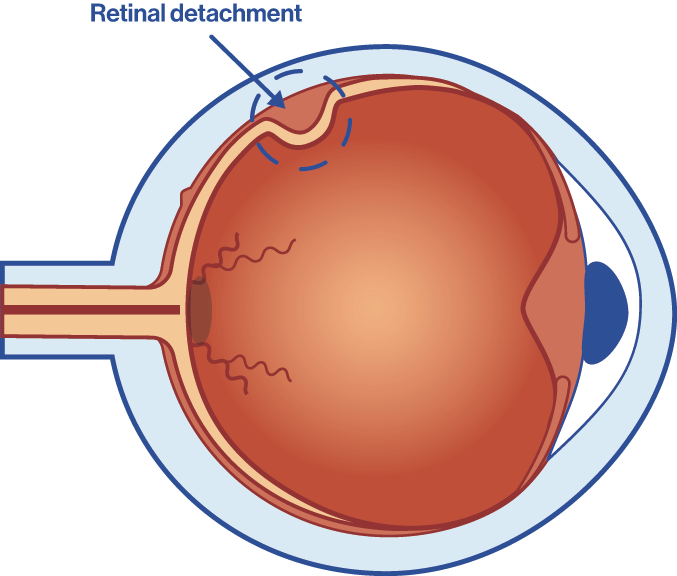
Retinal detachment is one of the most common disorders we encounter at Oftalvist’s Retina and Macula Unit. It occurs when the neurosensory retina (internal layer of the retina) separates from the pigment epithelium (external layer of the retina) due to a build-up of liquid between the two elements. As a result, part of the eye’s vitreous humour leaks into the area between the detached retina and the choroid, preventing the retina from repositioning itself correctly. The first and primary symptom is blurry vision.
The frequency of this disorder, mainly rhegmatogenous retinal detachment (the most common), is estimated at 1 in 10,000 people per year. Furthermore, while it usually affects men and women at equal levels, men between the ages of 50 to 70 tend to suffer from it more, as do people with myopia.
If left untreated, the retinal detachment will lead to full loss of vision in that eye (blindness), so it requires immediate treatment. Early diagnosis and treatment is key to limit the damage of this disorder in the majority of cases.
Types of retinal detachment
Rhegmatogenous retinal detachment
90% of retinal detachment cases seen in consultations fall within this category and it occurs as a result of a retinal tear or hole. It is usually more common in people with myopia, when they suffer some injury or after intraocular surgery. A family history of retinal detachment also increases the risk.
The patient will notice a severe but painless decrease in visual acuity that will seem like a curtain covering their visual field.
Traditional detachment
This type of detachment occurs when the patient suffers from a disorder at the vitreous interface where adhesion to the retina causes traction to be exerted on the retina by fibrovascular membranes.
Patients with untreated diabetic retinopathy tend to be more predisposed to this form, but it can also be caused by injury.
Exudative detachment
This is the least common type of detachment. It occurs when the retina becomes lifted due to exudation of liquid from the choroid.
This form of detachment is generally caused by a retinal or intraocular tumour, or by inflammation of the choroid.
Symptoms of retinal detachment
It is important to note that retinal detachment does not cause any pain in the eye, so anyone who suffers any of the symptoms mentioned below on a continuous and persistent basis should go to the emergency unit at an ophthalmology clinic.
Should one or several of the following symptoms arise, a specialist ophthalmologist will need to examine the retina through pupil dilation and ultrasound technology, to enable accurate diagnosis.
→ Blurry vision
This is the most common symptom, as when the retina becomes detached the patient’s vision will become blurry.
→ Flashes of light
The most common initial symptom of retinal detachment is flashes of light in your vision (photopsia), which will happen repeatedly in the same area of your visual field.
This may be a sign of a retinal tear and should be examined immediately.
→ Loss of central vision
When the macula is affected.
→ Floaters
Floaters (myodesopsia) look like small black dots that move around, and they are caused by changes to the vitreous.
→ Black curtain
The appearance of a dark curtain-like shadow in your field of vision that partially or fully blocks vision in one eye.
→ Distorted images
This is what ophthalmologists call metamorphopsia, a disorder where lines that should be straight under normal conditions are seen as wavy.
What are the main causes of retinal detachment?
The most common risk factors for retinal detachment, which usually occurs in both eyes, are:
→ Holes in the retina.
→ Choroid tumours.
→ Macular hole in patients who suffer from extreme myopia.
→ Complications from eye surgery, such as cataract surgery.
→ Eye injury.
→ Diabetic retinopathy.
→ Family members who have suffered from retinal detachment in the past.
Treatment for retinal detachment
The treatment for retinal detachment will always be surgical in nature and will depend on the degree of detachment. The specialist ophthalmologist will determine which technique is the most appropriate. There are several different techniques:
Laser photocoagulation
This may be effective in early stages, when holes are detected in the retina that increase the risk of detachment. Laser treatment applied to the retina by an expert at the right time may prevent detachment.
This treatment involves reducing or removing the abnormal blood vessels in the retina and, as far as possible, preventing the appearance of new abnormal vessels. It is primarily used on patients with diabetic retinopathy.
The surgery is performed using anaesthetic eye drops. The benefit of this treatment is that the laser beam is aimed directly at the affected area with great precision, preventing any burns to the surrounding area. The success of the treatment will depend on the severity of the problem.
After the surgery, the patient may notice that their vision has decreased temporarily, but it will come back within the first 2 to 6 weeks after the treatment.
Vitrectomy
Scleral buckling
Cryotherapy
Pneumatic retinopexy
Drainage of subretinal fluid
What is involved in retinal detachment surgery?
As a general rule, retinal detachment surgery involves repositioning and adapting the retina. However, in the most complex cases, the specialist ophthalmologist may opt for vitrectomy instead.

Repositioning the retina
The surgeon will push the wall of the eye out towards the retina by attaching a silicone band or belt.
Closing the tear that is causing the detachment
The surgeon will seal the edges of the tear with a laser or freeze treatment. This surgery may take the ophthalmologist 1 to 3 hours to complete, depending on the level of complexity.
What is the recovery like after retinal detachment surgery?
Since this is a particularly invasive form of surgery, the eye will be swollen after the operation, and the recovery will depend on the type of treatment used according to the level or the stage of the retinal detachment. The patient may also notice some pain or discomfort, but nothing too severe. Even if the problem has been resolved, the patient should be examined regularly to keep an eye on how the treatment is developing.
As in certain cases the patient’s eye will be filled with air, gas or oil with silicone, they should lie on their back when they sleep for approximately a month after the surgery.
If silicone oil has been used, a second procedure may be required a few months later to remove it.
How long is the recovery time after retinal detachment surgery?
The patient will generally fully or partially regain their vision over the course of 6-12 months after the surgery, depending on the severity of the detachment treated.
In the meantime, the patient will be prescribed specific antibiotic and anti-inflammatory medication and will be advised to keep their head in a certain position and avoid flying, particularly if the technique used was a vitrectomy.
Once they have healed, the patient will still need to be examined regularly to ensure that the treatment is developing correctly.
The treatment is exclusively surgical, via injection of gas into the eye, fitting of a band or a buckle, or a vitrectomy.
Preventing retinal detachment
The specialist ophthalmologist will recommend an annual check-up for patients at risk of retinal detachment, which will consist of the following:
→ Visual acuity test.
→ Checks for a change in the number, size and movement of floaters.
→ Full inspection of the retina with pupil dilation and a comprehensive examination of the periphery of the retina with different types of examination lenses, looking for possible ominous signs or predisposing lesions.
→ Annual check-ups for people with first-degree relatives who suffer from eye disorders such as diabetic retinopathy or magna myopia, which may increase the likelihood of retinal detachment.
→ Eye protection for contact sports or certain types of professions where there is a risk of eye injury from some kind of material or work tool.
Preventive laser treatment may also be advised for lesions that could trigger retinal detachment. As such, early detection will lead to more effective treatment and recovery. Speak to our retinal and macular specialists at Oftalvist for more information.